As someone who lives with diabetes, you know that it’s important to meet your doctor regularly. That includes meeting a diabetes specialist called an endocrinologist.
Although these types of bookings vary in frequency, they usually follow a quarterly HBA1C test.
Usually, diabetics see endocrinologists at least once a year to renew their management, blood work follow-up, and prescribing drugs such as metformin and insulin. It is best to prepare to make the most of these appointments.
This article provides an overview of 10 important questions to ask your endocrinologist next time you have an appointment.
Please prepare before booking
“Approach it like a well-run job to make the most of your visit with your endocrinologist,” said Dr. David Lamb, medical director of the Sinai Mountain Medical System’s Clinical Diabetes Institute.
Before meeting your doctor, bring a pen and notepad with your personal agenda written down.
“You and your doctor should be on the same page about your main concerns,” says Lamb.
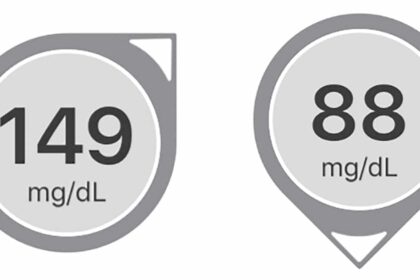
It is also important to bring blood glucose data from a continuous glucose monitor (CGM) or glucometer. Many phone apps can also share this data directly with the endocrinologist’s office.
10 Good Questions to Ask Your Endocrinologist
Does my diabetes control my goals well?
Everyone with diabetes is different, but it is very important to know how your diabetes management stands in comparison to your goals.
Endocrinologists usually order blood tests before an appointment. This includes the HBA1C test, which measures the average blood glucose level over the past three months.
Ask your endocrinologist this question directly. Perhaps you are planning on getting pregnant in the near future and trying to understand whether you need a much lower HBA1C or why you have a lot of hypoglycemia.
Whatever your diabetic goals, make sure they fit your current stage of life.
Does the rest of my blood work look normal?
A typical complete laboratory assessment measures HBA1C or higher. This thorough blood test measures thyroid function if you have urine, vitamin D levels, cholesterol (HDL and LDL), white and red blood cell count, and many other levels to check in your overall health.
When any of these levels are out of range, markers of Hashimoto’s disease, anti-syloglobulin antibodies (TGAB), and tissue transglutaminase antibodies (TTG-IGA), among others, are tests that test positive in approximately 98% of patients with celiac disease.
Both Hashimoto and Celiac are common in people with type 1 diabetes.
Do I need to adjust my diabetic medication and/or insulin?
If you are experiencing a lot of hyperglycemia and/or hypoglycemia, suffering from the dawn phenomenon, or are constantly high or low after eating or exercising, this is the perfect time to dig deep into the heart of diabetes management with your endocrinologist.
Based on the latest blood glucose data, endocrinologists can help them fine-tune their management by adjusting correction factors, insulin sensitivity, insulin-carbohydrate ratios, and basal rates.
This is especially useful if you have recently changed your lifestyle habits, such as diet or exercise routines, or if you are pregnant or planning to get pregnant.
How can I adjust my care between visits?
Meeting and asking questions about a doctor consists of less than 1% of the time you live with diabetes and you need to know what to do on the spot if you have problems.
You are sick and say you need to significantly increase the amount of insulin you are taking and you need to train for a marathon and suddenly become very insulin sensitive.
This is the ideal time to ask your endocrinologist when and how you can adjust your insulin dose and modifiers.
It can also help you know how your doctor’s office is available. Can I contact you during the visit for prompt guidance or advice? Will they answer the phone over the weekend? Do they use the Patient Portal email, text, or use? How can I get there in an emergency?
These are all great questions to ask and are definitely things you need to know for optimal care.
What new insulins, medicines and technologies are on the horizon?
New insulin is constantly hitting a market that functions better and faster than the best available five years ago.
These include Lumjev, Semglee, Tresiba, and Fiasp. Have you heard of them? Ask your endocrinologist about the latest insulin available and see if there are free samples you can try.
In addition to Dexcom’s G7 CGM, which will be coming later this year, patients are looking forward to Omnipod’s Horizon system for automated insulin delivery in 2021.
Trying out a new type of insulin or the latest technology means the difference between uncontrollable blood sugar and HBA1C that you are truly proud of, but you will never know until you try it!
Are there any other medications I should be?
Insulin may not be enough. The “unlabeled” of precision medicine and prescription drugs is extremely popular in the diabetes field.
Sometimes people living with type 1 diabetes need insulin and metformin to thrive. People with type 1 diabetes are also prescribed SGLT2 inhibitors that help manage insulin resistance and weight gain.
Popular drugs among type 1 people are Symlin and Victorza. Daily injectable prescription drugs that “mimic” the activity of GLP-1 is the activity of intestinal hormone (incretin), which induces insulin secretion from beta cells by binding to the pancreatic GLP receptor.
This helps you feel full after eating, excessive hunger, weight gain, and insulin resistance. Ask your doctor if it might be correct for you to add supplemental prescription medications to your insulin regimen.
How can I afford to buy medicine?
The truth is, one in four people with diabetes in the US pays insulin just at the cost. People are struggling and insulin is expensive. Today’s Humanlog vials cost over $300, but when they were introduced to the market in 1996, the same vial cost is $21.
If you are struggling to afford your medicine, you are not alone. Ask your doctor about how you can better buy your medication.
Perhaps you are eligible for your state Medicaid, or a tax subsidy health plan for your state exchange.
Perhaps you are eligible for reduced or free insulin at a federally qualified health center that will participate in the 340B program.
There is probably a nationally regulated health plan subject to the state’s co-payment cap law. Alternatively, you can seek assistance from a drug manufacturer.
Ask about the resources to get the help you need. Help is there, you need to let your needs know.
How can I better manage my diet?
Diet is the foundation of diabetes management, and it is important to check in your nutrition regularly. Check with your doctor about your regular diet plan and ask for your opinions on foods that may need to be added or subtracted.
The food is often tasty, but it may not serve you or your diabetes well and you may know an alternative that you can try instead.
This is also a good time to mention any issues you may have with eating, as diabetic youth are almost twice as likely as people without diabetes.
If necessary, an endocrinologist can write an introduction to see registered nutritionists to help you polish your diet better if you are sugar cravings, emotions, or dealing with excessive weight gain or fatigue.
How can I exercise safely and effectively?
Exercise is important for good diabetes management, but it is not always easy to stay motivated. Talk to your endocrinologist about new exercise ideas for inspiration.
Perhaps you need suggestions on how to make your running routine winter into winter, or you need fresh ideas to recover from excessive injuries.
You may also be exercising for the first time, or you may be suffering from extreme highs and lows afterwards. Ask your endocrinologist how to better regulate your food intake and insulin for exercise to thrive.
According to the Centers for Disease Control and Prevention, adults should aim for moderate exercise for 150 minutes a week. Or, for about 30 minutes on most days, work with your doctor on how to reach at least that amount of exercise each week.
What can you do now to prevent complications?
If HBA1C and general diabetes management do not match your goals, it’s time to develop an action plan with your doctor. Ask what you can do today to prevent future complications.
Maybe they’re switching their morning routines to suit their normal walks. You might cut out the sugar added on weekday nights or mention the fast food completely. Whatever your advice is, make sure you can stick to it and make sure it fits your lifestyle and long-term goals.
The best time to begin preventing diabetes complications is always yesterday. The next best time is now.
Bring these questions and ideas to the next appointment of the endocrinologist and make the most of your (and your physician) time. Evolving diabetes management starts with asking good questions, so make sure you’re ready and ready to be in charge of diabetic health!