Anyone can experience a diarrhea attack with or without diabetes, but for some people it can be a direct result of diabetes.
Also known as “diabetic diarrhea,” this is one of the lesser known complications of diabetes, but it is extremely difficult to manage and live daily.
It is estimated that about 22% of people who have lived with diabetes for a while will experience diarrhea frequently.
In this article, we will look at the causes, symptoms and treatment options for diabetes-related diarrhea.
How does diabetes cause diarrhea?
Diabetic diarrhea can be the result of long-term hyperglycemia levels that damage nerves and overall function in the colon, small intestine, and stomach (a condition known as neurological disorders).
“Many gastrointestinal complications of diabetes appear to be related to dysfunction in the neurons that supply the enteric nervous system,” explains the 2000 edition. Clinical diabetes.
Damage to nerve fibers throughout the digestive system can cause constipation or diarrhea (often both) at different times, as some nerves stimulate movement and others help to slow the movement of the intestine.
The diarrhea attack is ongoing or lasts for months and can be quiet for several months. The diarrhea stage can also be countered by constipation stages.
Another possible cause of diabetic diarrhea is that people with diabetes are more likely to consume large amounts of artificial sweeteners and sugar alcohols known to be powerful laxatives.
Diagnosis of diabetic diarrhea
There is no easy way to test and determine whether the cost of your symptoms is related to nerve damage or something.
If you think diarrhea is directly related to diabetes, schedule an appointment with your medical team and pay attention to the frequency and severity of your bowel movements for a week or two.
Depending on their assessment, your healthcare team may refer you to a gastroenterologist for further investigation.
Treatment Options
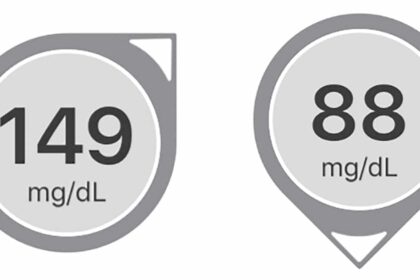
First of all, working with your healthcare team to improve your blood sugar levels is an important part of treating diabetic diarrhea.
Without dealing with blood sugar levels, you continue to experience nerve damage throughout your digestive system (and your whole body) and experience unpleasant symptoms.
Secondly, your doctor may advise you to change your dietary habits. You may need to eat more fiber (or less fiber), drink more water, or include more (or less) vegetables in your diet.
Finally, several specific medications have been used to help patients deal with the effects of this nerve injury and reduce or eliminate diarrhea attacks.
- Parenteral somatostatin analog octreotide: This option has proven useful in patients with long-standing diabetes and digestive complications. This is an injectable medication that is mainly used to treat different types of diarrhea.
- Selective serotonin 5-hydroxytryptamine type 3 (HT3) receptor antagonist: This is one type of 5-HT3 agonist and is useful in treating diarrhea. It can be useful for extreme nausea and vomiting, recurrent diarrhea, or diarrhea associated with chemotherapy.
- Basic over-the-counter treatment: There are a variety of over-the-counter options to treat common diarrhea, but it is not likely to work in diabetic patients suffering from severe nerve damage to the colon and the entire digestive system.
Other possible causes of diabetic diarrhea
Aside from neuropathy in your colon, there are a few things to consider when assessing the potential causes of gastroenterological calamities.
Metformin
Metformin is one of the most prescribed drugs in the world and is the first line of treatment for people with type 2 diabetes, but it can undoubtedly disrupt the digestive system.
In fact, the need to “run to the toilet” frequently while taking metformin is one of the reasons why many patients stop taking it completely.
The biggest thing you can do to manage diarrhea caused by metformin is to talk to your doctor about getting more expensive “extended release” version of your insurance.
This is not the first version due to its costly cost. So try the cheaper version of health insurance first.
If you report side effects and your doctor document this, you are more likely to get insurance approval for an extended version of metformin.
“Low Carbohydrate” Products with Sugar Alcohol High Diet
If you’re eating lots of low-carb protein bars, candies, ice cream and other processed products that use sugar alcohol as a sweetener, don’t be surprised if you run to the toilet regularly.
Sugar alcohol is a known laxative. While most people can consume sugar alcohol without digestive issues, most people will find themselves dealing with stomach cramps, gas and diarrhea too often.
Everyone has different tolerance levels for sugar alcohol. Beware of these types of products, and pay attention to how your body reacts to different types of sugar alcohol, and how often you eat it.
Celiac disease or gluten intolerance
Although not as common as other conditions often associated with diabetes, celiac disease or gluten intolerance occurs frequently enough in the diabetic population and should allow for that to anyone with diabetes.
Celiac disease is an autoimmune state. This means that when gluten is present, the immune system starts attacking your body. This can be tested with a simple blood test, but don’t start eating a “gluten-free diet” rear You’ve done a test. Otherwise, your results may not show signs of celiac disease.
Gluten intolerance is like an allergy. Eating gluten makes you feel terrible in many ways. The only way to “test” this is to completely remove gluten from your diet for at least 3 weeks, assess whether the symptoms are gone, and then reintroduce it to assess whether symptoms will return.
Symptoms of either condition include headache, enlargement, gas, fatigue, diarrhea, depression, brain fog, skin problems (e.g. eczema, acne), weight loss, constipation, or penetrating stools with dirt.
Yeast infection in your digestive tract
People with consistently high blood sugar levels face significant risks of yeast infections, including the gastrointestinal tract. This overgrowth of yeast is a direct result of too much glucose in the bloodstream.
These areas of the body require yeast and bacteria, but when blood sugar levels are consistently high, excess glucose feeds the growth of the yeast.
In most cases, after being tested by a doctor, antifungal drugs such as nistatin, ketocanazole, or flucanazole are prescribed to kill excess yeast.
Fortunately, this treatment is extremely effective and can resolve most yeast infections within a few days to a week. However, please remember some of the treatment plans Must do Include work to improve blood sugar levels. Otherwise, you simply develop another yeast infection.
Irritable bowel syndrome
Irritable bowel syndrome (IBS) is a comprehensive diagnosis of a variety of gastrointestinal symptoms. It appears to be more common in the diabetic population, but it can develop in anyone.
Symptoms of IBS can include two specific details.
- Continuous abdominal pain
- Frequent changes in bowel movements (diarrhea, constipation, or both)
- Discomfort after eating (although consistent foods cannot be specified as the cause of pain)
- Bloody and gas
- Difficulty sleeping due to overall discomfort
Testing IBS is difficult. Instead, the diagnosis is usually the result of excluding other options, especially celiac disease and gluten intolerance. In people with diabetes, nerve damage in the colon and small intestine is also frequently considered.
Diagnosis of IBS is generally the result of cases where it is clear that there are no other signs of damage or other conditions affecting parts of the digestive system.
Treatment of IBS can include some over-the-counter medications for constipation or diarrhea, but you probably need to take good notes about what food causes the most pain. You should consider removing gluten from your diet and improve the overall amount of many foods (processed foods).
For many people, following the “low-fodmap diet” can be extremely helpful in improving IBS-related symptoms.
Probiotics – With the support of a doctor, it can also help improve beneficial bacteria in the gut, and help improve digestion.
Stress can also play a major role in IBS. If you are experiencing significant stress in your life, consider this as a potential cause of digestive upsets and talk to your medical team about changes in your life to reduce stress and anxiety.
Simple steps to improve digestive health
As people with diabetes are common, digestive issues – but there are many things you can do to prevent and protect yourself, starting with improving your blood sugar levels. generally Whole Foods and regular exercise.
Don’t forget to spread a cigarette and limit alcoholic drinks several times a week rather than every night.
Like many aspects of diabetes health, improving and protecting digestion comes down to the simplest habits and choices we make every day.
Suggested next post:
If you find that Diabetes Diarrhea Guide is useful, please use the form below to sign up for our newsletter (and get the free chapter from Diabetes E-Book Fit). We will send you a weekly newsletter with the latest posts and recipes from diabetes.