Do you have a hypoglycemia program?
When living with insulin-dependent diabetes, hypoglycemia is an inevitable part of life, and is always prepared by consuming carbohydrates such as glucose tablets and juices.
However, hypoglycemia can creep up dangerously low. So you should also be prepared for severe hypoglycemia or situations where you can’t eat more carbohydrates.
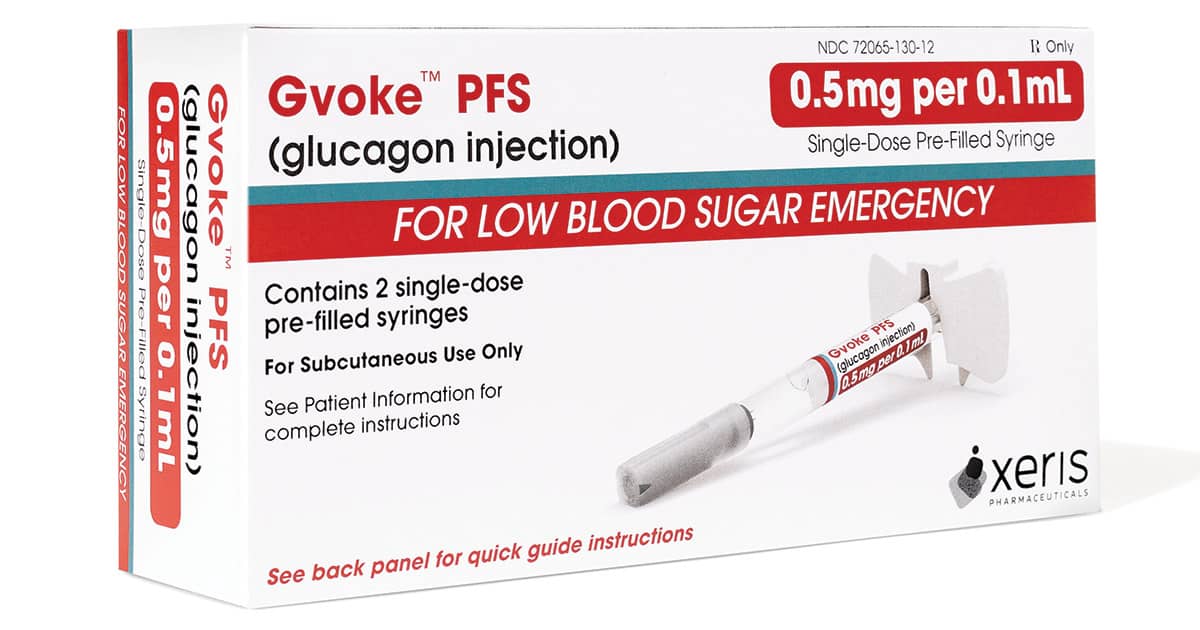
Historically, there have been very limited options when it comes to treating these horrible, severe low levels, but glucagon, which was first filled with Gvoke® (glucagon injection), was now available, and ultimately there were options available for immediate use.
I had the opportunity to sit down with Paloma Guerrero (aka Glitterglucose), who has been living with type 1 diabetes since 2013, to discuss experiences of severe low levels and how to properly prepare for an extremely low blood sugar emergency.
This post is by Xeris Pharmaceuticals, Inc. is sponsored by. Manufacturer of GvokePypen® (glucagon injection).
What is hypoglycemia and why is it scary?
Hypoglycemia (hypoglycemia) can feel different to different people both when we feel low and how our symptoms appear.
In a non-diabetic body, blood glucose levels are rarely soaked below 70 mg/dL, but insulin (or other low-glycemia drugs) manage diabetes, and if there is too much insulin in the body, blood glucose levels start to fall below normal levels.
Without sufficient glucose (the sugar form) in the bloodstream, the brain and whole body struggle to function, and most people start to feel symptoms of hypoglycemia.
If not treated with glucose, blood glucose levels may continue to drop, leading to severe hypoglycemia. Severe hypoglycemia is defined as a situation where blood glucose levels are very low, so you need help from someone else to return your blood glucose to a safe range.
The Story of Paloma
Using the glucagon kit was not the best mind for Paloma until he experienced two very bad hypoglycemia that was only a week apart. In one situation, she was ready, and one thing wasn’t.
For the first time, she was on a road trip with a friend. She brought all the diabetes items, including Gvoke. Her friend knew where it was and how to use it.
Once they arrived at the hotel, Paloma checked her CGM and saw that she was 179 mg/dl (9.9 mmol/l), but within the next hour she began to feel low. She was shaking with sweat. She checked her CGM again, and now her blood sugar level is 52 mg/dL (2.9 mmol/L), and the CGM shows an arrow downwards, indicating a drop in blood sugar levels.
She began eating the urgent low snacks, but this low low felt differently and her blood sugar levels continued to drop, so she began to fear she would faint. At that point, her friend got a Gvoke for her. Paloma injected it into her thighs, taking medications that have been proven to cause blood sugar, and felt a sense of security to know that she was fine.
Her blood sugar levels rose steadily, topping at 237 mg/dL (13.2 mmol/L) and then sedimented at 180 mg/dL (10 mmol/L).
Gvoke is a suitable tool for that situation, fixing her low without putting her on a 24-hour blood sugar coaster.
What happens when you can’t prepare for hypoglycemia
The following week, Paloma and her friends were on their way again. This time she didn’t bring in Gvoke (I didn’t think I needed it for two weeks in a row), and there was a tendency to be low during the trip, so she ate all of her low snacks before arriving at the hotel.
That night, she woke up and checked her CGM and found that her blood sugar level had dropped to 40 mg/dL (2.2 mmol/L). However, she had no snacks and no glucagon with her, so there was no way to treat the low ones.
Her friend ran to a vending machine in the hallway, which was malfunctioning. Time was chocking in, and her friend punched the glass of the machine to reach the snacks.
At this point they both panicked and Paloma ate as much as they could after her friend returned with a snack. This experience evaporated them emotionally and she had to fight against highly resistant blood sugar the next day.
How these experiences have changed how she prepares for hypoglycemia
Both serious low situations were scary, but I felt more controlled and less emotionally exhausted, knowing that she was receiving the correct treatment with her, despite her most aggressively lowering blood sugar levels during the first episode.
It was premixed and ready to go without visible needles, so she wasn’t nervous about whether her friends could use it if she needed help.
She made some changes to her care after two low episodes, but is currently wearing a new CGM model that warns if her blood sugar levels fall below range. She also has a Gvoke Hypopen all the time, telling people around her where it is and is sure that people around her can use it if they need it.
I asked other people who live with diabetes if they have advice words and this is what she said:
“An emergency will occur. Even if we think it will never happen to us, we will do so sometimes, so preparation for such a situation is very important. And the problem is, if we are prepared and have the right solution with us, we don’t need to scare hypoglycemia. For me, knowing that Gvoke works, it’s ready to use, not destroying my blood sugar means a world of difference and now I don’t go anywhere. ”
What is Gvoke Hypopen?
Gvoke Hypopen can be used to treat severe hypoglycemia if you or someone around you experience one or more of the following:
- I’ve tried repeatedly to fix it with food and drinks, but it’s not working
- Can’t swallow safely
- You/I feel like they might faint
- Experience loss of consciousness or seizure
Gvoke is the only predicted glucagon approved for children over two years, and there is no need to worry about measuring glucagon doses as Gvoke is two pre-measured doses. Adolescents and adults (1.0 mg), one for ages 2 and older (0.5 mg).
Children under the age of 12 who are at least 100 pounds in weight are prescribed a dose of 1.0 mg.
Gvoke is a prescription drug, so you need to reach out to your doctor and request a prescription. If you have commercial insurance, you can also request that you pass directly through gvokeglucagon.com and provide a prescription directly to the door.
For a limited time only, Xeris Pharmaceuticals will provide $0 Copay to commercially eligible patients to ensure as many people as possible have access to Gvoke Hypopen.
—————
Important Safety Information
Gvoke is a prescription drug used to treat very hypoglycemia (severe hypoglycemia) in children and children with diabetes who are older than 2 years old. It is unclear whether Gvoke is safe and effective for children under the age of 2.
Do not use Gvoke if you have a tumor in the gland above the kidney (adrenal gland), known as a nephrocytoma. There is a tumor in the pancreas, called insulinoma or glucagonoma. You are allergic to glucagon and other inactive ingredients in Gvoke.
Gvoke can cause serious side effects, including hypertension. Gvoke can cause hypertension in certain people with tumors in their adrenal glands. Hypoglycemia: Gvoke can cause hypoglycemia in certain people with tumors in the pancreas. Serious Skin Rash: Gvoke can cause serious skin rashes in certain people with tumors in the pancreas called Glucagonoma. Serious Allergic Reactions: If you have a serious allergic reaction, such as rash, difficulty breathing, or hypotension, call your doctor or get immediate medical assistance. US-SM-GVKHP-21-00081
See important safety information: http://bit.ly/2ljdbjy
Full prescribing information: see http://bit.ly/2lrtk07












