When I was diagnosed with type 1 diabetes 22 years ago, I didn’t expect a tubeless automated insulin delivery (AID) system to be possible.
At age 12, I was handed a syringe, several vials of NPH and R insulin (pork insulin) and told to test my blood sugar levels more than 10 times a day and expect the best. It was brutal.
Decades later, technology has come a long way, to say the least.
You can remotely bolus the insulin and look down at your smartphone to seamlessly check your blood sugar levels. With the latest Omnipod 5 system, you won’t be too worried about low blood sugar levels if your blood sugar levels are high.
The system automatically adjusts my basal insulin rate for me, depending on what my blood sugar is.
In this article, I will explain the new Omnipod 5 system, my first impressions, and what you can expect if you choose this system yourself.
Short History of Automated Insulin Delivery (AID)
Automated insulin delivery, or aid for short, has been the holy grail of the diabetic community and has long been the holy grail.
Even with traditional insulin pump therapy, people with insulin-dependent diabetes often walk on tightropes that manage their stubborn heights and horrible lows, often feel imprisoned by blood sugar levels.
Aid hopes not only minimizes highs and lows, but also reduces the mental burden of life that has lived with diabetes.
People with diabetes in the #WearEnotWaiting movement have hacked years of old insulin pumps to achieve hybrid crop loop systems, but these have never been approved by the Food and Drug Administration (FDA), not recommended by doctors, and no safety guarantees.
The first system approved by the FDA, the Medtronic 670G, became available in the US in late 2016. The system automatically adjusts basic delivery based on Guardian, Medtronic’s proprietary continuous glucose monitoring (CGM) system, and was extremely popular.
The TSLIM Control IQ system, which became available in the US in early 2020, quickly followed from tandem. This is a first aid system to work with the Dexcom CGM system and did not require fingertip calibration (unlike the Medtronic system, which requires calibration every 12 hours).
The Guardian CGM had to be changed every 7 days, but the TSLIM system using Dexcom CGM required changes every 10 days.
People were very excited about these systems, but millions were embracing hope for the (at the time) Omnipod horizon system by Insulet.
This system is unique in the fact that it will all become the first tubeless aid system operated by Bluetooth.
Many people prefer the Omnipod system because they lack tubes, giving them the freedom to exercise and feel more free. Also, there is no need to hang insulin when you are in the shower or swimming.
The Horizon system, now known as the Omnipod 5, was scheduled to be approved by the FDA in 2020, but the Covid-19 pandemic quickly caused a major bottleneck in the approval process, which was repeatedly delayed.
Finally, on January 28, 2022, the FDA announced approval for the Omnipod 5 system. The approval is for people with type 1 diabetes over the age of 6 and is compatible with Android smartphones and Dexcom G6 CGM systems.
Insulet will release a limited release in February, and a market release was expected in March 2022.
How Omnipod 5 works
It is important to note that this is a hybrid crop loop system and users need to count carbohydrates and bolus insulin for every meal or snack.
You also need to let the system know when you are planning your exercise. It also has an activity feature that allows you to reduce your insulin needs while you are physically active.
However, the aid system automatically adjusts the basal insulin rate according to your blood glucose level 24 hours a day according to your blood glucose level.
The system is similar to previous versions, working with Dexcom G6 CGM, which requires the pod to be replaced with insulin every 72 hours and filled with insulin, and every 10 days.
My first impression
I was lucky enough to be part of a limited release group and received the Omnipod 5 system on February 11th, 2022.
My first impression was that my personal diabetes manager (PDM) looked like a smartphone (it’s probably one), and the pod (self-contained insulin reservoir) was very similar to the earlier versions of the Omnipod (both the Eros and the Dash Use Pod).
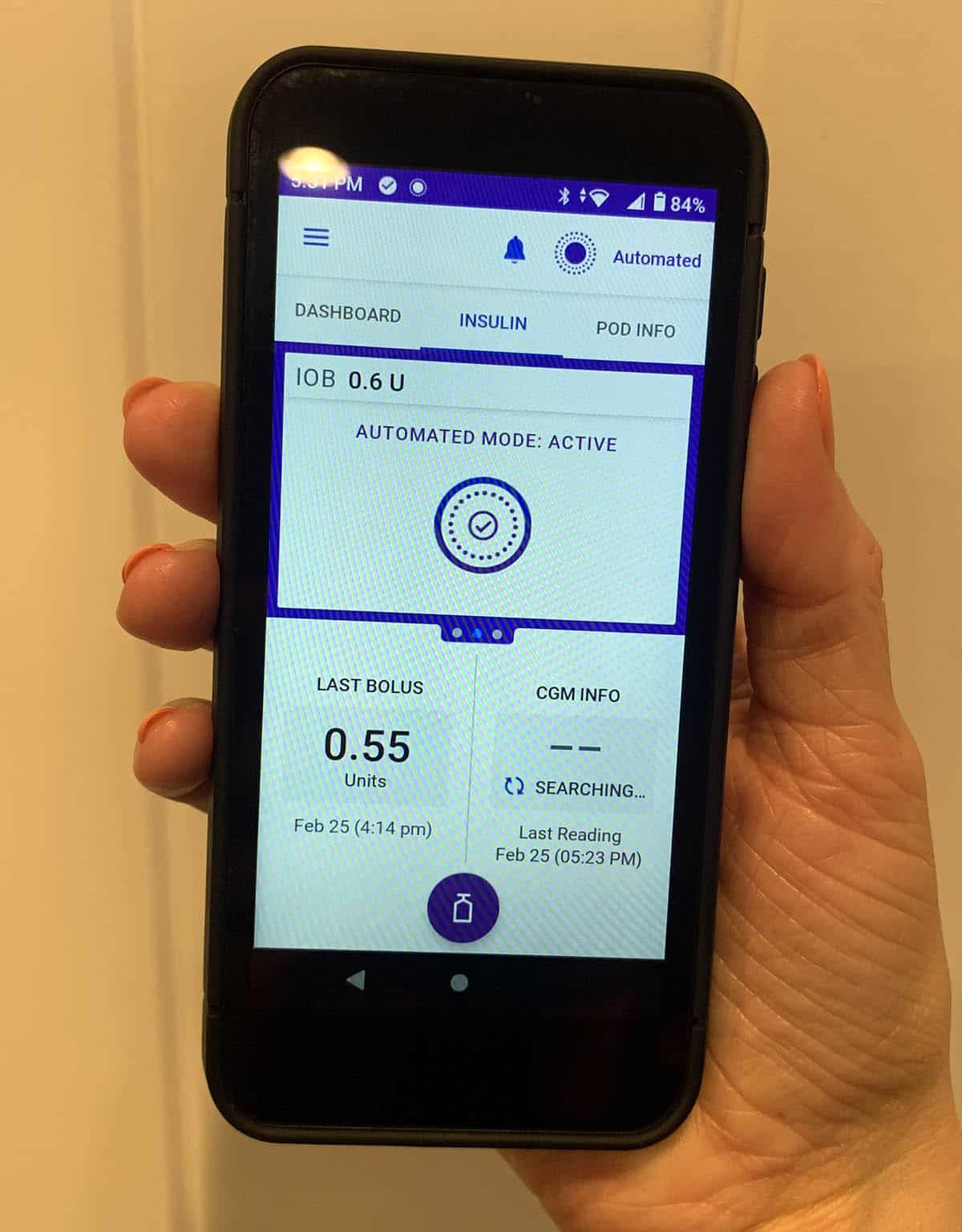
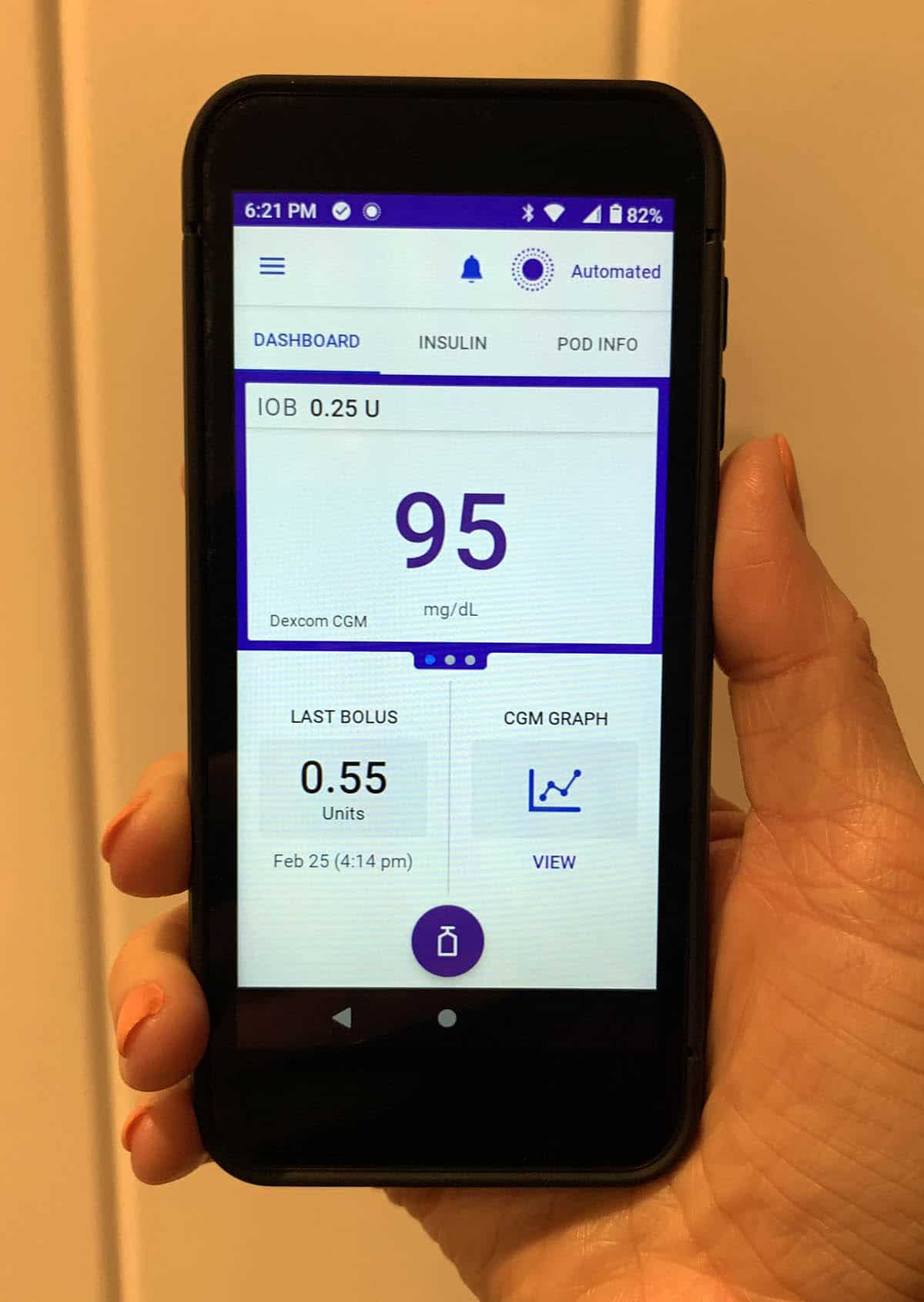
PODs are now “talked” to Dexcom CGM sensors. So, even if the PDM is not nearby, the basal rate will be automatically adjusted (required only near the bolus). Or, if you use an Android phone, there’s a compatible app that you can use for PDM instead, and a bolus directly from your smartphone (how cool is that?!). Since I’m using an iPhone, I chose the traditional PDM.
There is a saying that iPhone compatible apps are approaching.
I had a 2 hour training session and immediately jumped into automatic mode (why do I wait?). It was amazing.
I was only in the system for two weeks, but I have already noticed some significant improvements in my health.

The quality of sleep has been improved
After switching to automatic mode, I quickly folded, ate, and got my bed ready for a regular dinner.
Like many people with diabetes, I didn’t always get much sleep at night. Between hypoglycemia and hyperglycemia and the accompanying alerts and alarms, I often wake up one or four times at night.
If I’m not awake to the alarm, I usually feel thirsty or at least need to pee once. So when I woke up the next morning, I was able to stay ecchi without interrupting my 8 hours of solid sleep.
I looked at the Dexcom graph briefly and found that my blood sugar level stayed between 110 and 130 all night.
Most of my nights look like this now, and the feeling of full rest is incredible. It’s a complete joy to feel like diabetes isn’t stealing my sleep as much as it used to be. And sleeping all night is definitely something I look forward to getting used to!
Less confusion in the exercise
I am an avid athlete who exercises 6-7 times a week. I love running, hiking, swimming, cycling and weightlifting, and one of the most frustrating aspects of diabetes is how often hypoglycemia gets in my way.
I also hate having to eat before exercising. Because if I’m trying to lose weight, I sometimes feel like I’m beating my purpose.
I went low almost every day while exercising. Well, since I was with Omnipod 5, I have suffered one hypoglycemia in two weeks wearing the device. One!
This system allows you to set the target blood glucose level (in my case I would set it to 150 mg/dL), reducing the basal velocity (or pauses insulin delivery) until you can predict that it will reach that altitude.
You can set the 1-24-hour time to engage in the “Activity Function” and it will expire automatically.
Set the activity feature to “ON” every day approximately 45 minutes before starting your exercise routine. It will increase your blood sugar level smoothly and ensure that it does not crash. That’s amazing.
Less mental strain
Overall, being on Omnipod 5 eased my mental burden of living with type 1 diabetes.
In one study, diabetics add 180 decisions almost daily just to properly care for themselves, and having an aid system feels that those decisions have been reduced in half.
There is no need to micro-manage the basic rate during the day. I haven’t woken up a low alarm in the middle of the night to pause my insulin and eat some juice. I’m sleeping better than ever before.
Exercise is easy (and I can exercise without fear of finally getting low!).
And while it feels the same as usual when you administer insulin for your diet (you have to count carbohydrates and bolus for your meals and snacks), I know that refilling carbohydrates to prevent highs, or reducing insulin if you take it by chance and take it by chance, will replenish additional basal insulin in your system.
Diabetes is always a mental burden on those who live with it (and their families!), but having an aid system reduces that burden significantly.
Conclusion
Although the automated insulin delivery (AID) system is not yet a treatment for diabetes, we found that the Omnipod 5 system has significantly improved sleep quality, motor skills, and reduced the mental burden experienced as a woman living with type 1 diabetes.
However, it is still an external medical device. You can experience bad pump sites, blockages, infusions into scar tissue, and failed adhesives.
It can cause high blood sugar levels and both hypoglycemia levels, which can significantly improve your sleep quality, but you probably need to pee from time to time in the middle of the night. CGMS exerts errors and provides incorrect readings.
Literally, your “pancreas” every night (battery can last an average of 48 hours), and if there is no power for a long period of time, the battery may run out.
There’s nothing perfect. But while we are constantly waiting for the evasevasevasive Cure, this is a step closer to it.












